Uterine Artery PI
First Trimester Examination of the Uterine Artery Doppler
Pre-eclampsia, which affects about 2% of pregnancies, is a major cause of perinatal and maternal morbidity and mortality. Routine antenatal care has evolved with the aim of identifying women at high-risk for subsequent development of pre-eclampsia. The likelihood of developing pre-eclampsia is increased by a number of factors in the maternal history, including Afro-Caribbean race, nulliparity, high body mass index and personal or family history of pre-eclampsia. However, screening by maternal history may detect only about 30% of those that will develop pre-eclampsia for a false positive rate of 10%.
A more effective method of screening for pre-eclampsia is provided by uterine artery Doppler at 11+0 to 13+6 weeks’ gestation in combination with maternal history. For a false-positive rate of 10% the predicted detection rate of pre-eclampsia requiring delivery before 34 weeks is 80%, compared to 30% for late pre-eclampsia. This is particularly important because it is early rather than late pre-eclampsia which is associated with an increased risk of perinatal mortality and morbidity and both short-term and long-term maternal complications.
Identification of women at high-risk for PET during the second-trimester could potentially improve pregnancy outcome because intensive maternal and fetal monitoring in such patients would lead to an earlier diagnosis of the clinical signs of the disease and the associated fetal growth restriction and avoid the development of serious complications through such interventions as the administration of antihypertensive medication and early delivery.
It is imperative that, as for the NT scan, sonographers undertaking risk assessment of pre-eclampsia by examination of the uterine arteries must receive appropriate training and certification of their competence.
Protocol for the first trimester examination of the uterine artery Doppler
- The gestational age must be 11+0 to 13+6 weeks.
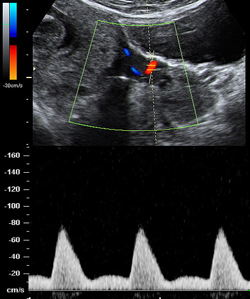
- Sagittal section of the uterus must be obtained and the cervical canal and internal cervical os identified. Subsequently, the transducer must be gently tilted from side to side and then colour flow mapping should be used to identify each uterine artery along the side of the cervix and uterus at the level of the internal os.
- Pulsed wave Doppler should be used with the sampling gate set at 2 mm to cover the whole vessel and ensuring that the angle of insonation is less than 30º. When three similar consecutive waveforms are obtained the PI must be measured and the mean PI of the left and right arteries be calculated.