Tricuspid Flow
First Trimester Examination of the Fetal Tricuspid Flow
The findings of recent studies suggest that examination of the fetal tricuspid flow at 11-13+6 weeks could have major beneficial implications in screening for Trisomy 21 by maternal age and fetal nuchal translucency (NT). However it is imperative that, as for the NT scan, sonographers undertaking risk assessment by examination of the fetal tricuspid flow must receive appropriate training and certification of their competence in performing the tricuspid flow scan.
This document describes the Fetal Medicine Foundation:
- Protocol for the assessment of fetal tricuspid flow
- Clinical application of tricuspid flow findings
- Certification in the first trimester assessment of the fetal tricuspid flow
Protocol for the assessment of fetal tricuspid flow
- The gestational period must be 11 to 13+6 weeks
- A four-chamber view of the fetal heart should be obtained
- A pulsed-wave Doppler sample volume of 2.0 to 3.0 mm should be positioned across the tricuspid valve so that the angle to the direction of flow is less than 30 degrees from the direction of the inter-ventricular septum. The angle correction tool must be utilized to show the angle of insonation relative to the inter-ventricular septum.
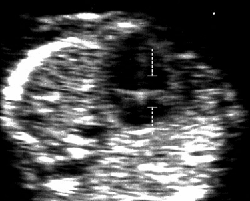
Apical four-chamber view of the heart at 12 weeks. The Doppler sample volume is positioned in the tricuspid valve orifice, including the right atrium and ventricle. The alignment of the atrioventricular valve flow is parallel to the ultrasound beam. - Tricuspid regurgitation is diagnosed if it is found during at least half of the systole and with a velocity of over 60 cm/s, since aortic or pulmonary arterial blood flow at this gestation can produce a maximum velocity of 50 cm/s.
Doppler flow profile in the tricuspid valve with no regurgitation during systole (a), and regurgitation during approximately half of systole and with a velocity more than 60 cm/s (b) The short reverse ‘spike’ generated by closure of the valve cusp (c) and the jet produced by aortic or pulmonary arterial blood flow, which at this gestation can produce a maximum velocity of 50 cm/s (d), should not be mistaken for tricuspid regurgitation. - The tricuspid valve could be insufficient in one or more of its three cusps, and therefore the sample volume should be placed across the valve at least three times, in an attempt to interrogate the complete valve
Clinical application of tricuspid flow findings
The incidence of tricuspid regurgitation is related to NT and CRL as well as aneuploidy, being more common with increased NT and smaller CRL measurements. Therefore it is not possible to give simple numbers by which the presence of normal flow will reduce the risk for Trisomy 21 and the presence of tricuspid regurgitation will increase the risk. The Fetal Medicine Foundation software includes tricuspid flow in the calculation of risks but access it available only to sonographers who have been appropriately trained and accredited in the assessment of the fetal tricuspid flow.
The software firstly calculates a risk based on maternal age, fetal nuchal translucency and maternal serum free beta-hCG and PAPP-A. If the risk is more than 1 in 50 and tricuspid flow is normal the risk does not change. If the risk is 1 in 50 to 1 in 1,000 and the tricuspid flow is normal the risk is usually reduced. If there is tricuspid regurgitation the risk is always increased. In addition, there is an increased risk for cardiac defects and therefore such patients should have a follow up specialist fetal cardiac scan.